Learning lessons from the COVID pandemic…we could do SO much better.
We must mitigate, vaccinate, and communicate...
The pandemic is at the back of many peoples’ minds as we “live with” SARS-CoV2. Yet, this belies reality as ongoing suffering adds to the dreadful toll paid for not controlling this virus (Fig1). It must never be as bad again as H5N1 avian influenza waits in the wings (pardon the pun).
Nevertheless, “normality” prevails so powerfully that we accept NHS winter (now perennial) pressures, despite knowing we CAN mitigate respiratory diseases. The previous Government pushed individual responsibility through staying alert and common sense to restore freedom. Yet this illusory policy leaves us at risk, whether “vulnerable” or “healthy” (yes, quotations are deliberate).
Public health should act at the population level, yet only the Green Party has a substantive COVID/respiratory infection policy. We must “mitigate, vaccinate, and communicate”.
1. Mitigate
The previous Government’s pendulum-like response created a false binary of “lockdown” vs. freedom. Delay and dithering as cases skyrocketed ultimately led to much harsher and longer restrictions, whilst unlocking too quickly drove yo-yoing prevalence and far higher deaths and hospitalisations than countries that controlled COVID, like South Korea.
Figure 1. Weekly deaths with COVID-19 on the death certificate by date of registration (Source UKHSA Dashboard).
Find, Test, Trace, Support, and Isolate (FTTIS) underpins infection control, depriving the virus of hosts within environments refractory to transmission, expertly practiced in Southeast Asia. Critically, FTTIS needn’t restrict freedoms, unlike initial UK COVID measures that eliminated seasonal influenza during 2020/21.
Knowledge is power, so testing is critical. PCR is costly, yet essential during the acute phase or healthcare settings, whereas LFDs provide excellent community insights. Wastewater surveillance provides near real-time prevalence, comparable genetic epidemiology to PCR, and is amenable to tracking multiple pathogens. However, UKHSA halted this in England during 2022.
Since 2010, the damage done to the NHS and dramatically worsening health inequalities have in turn affected how we are affected by the pandemic. This has been compounded by the abandonment of infection control in favour of futile drives to improve school and NHS staff attendances. Unsurprisingly, nosocomial SARS-CoV2 and other infections continue to blight hospitals and care settings. Means to combat airborne transmission of SARS-CoV2 and other viruses have been abandoned, including the wearing of well-fitted respirator masks, placing vulnerable patients at risk along with a lack of testing.
“Infection resilient” environments provide an excellent public health solution to these problems, removing the onus from individuals whilst reducing infection AND pollution. Improving indoor air quality by ventilation, filtration, sterilisation etc. would save £8bn annually, rising to £23bn during a pandemic according to the Royal College of Engineering. The CLASS-ACT trial showed that air filtration reduced overall absence from school by 20%, and a similar approach eliminated SARS-CoV2 and other pathogens from Addenbrookes Hospital. However, an absence of nationwide investment restricts best practice to venues such as the Davos WEF summit.
If the Sanitary act of 1866 was introduced after ~6000 died of cholera, surely losing almost fifty times that number to COVID since 2020 (>10K in the last 12-months) should motivate us to add clean air as a basic human right.
2. Vaccinate
A vaccines plus strategy fits the “Swiss Cheese” pandemic mitigation model for COVID or other infections. The notion that you should get infected to become immune to what just infected you is madness when effective vaccines are available.
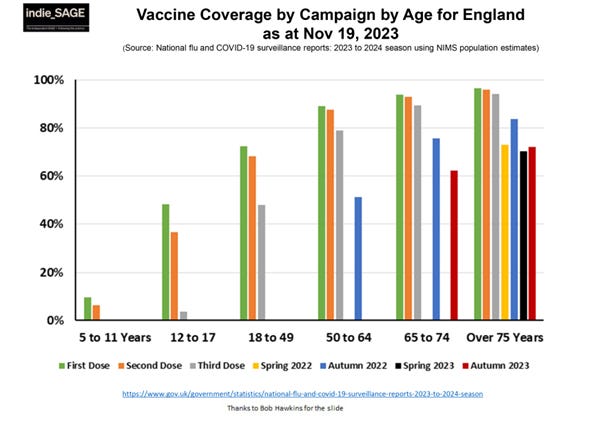
This was finally recognised by JCVI recommendations for childhood chicken pox vaccines, although this is yet to materialise. Juvenile vaccinations are down across the board and targeted vaccination doesn’t protect enough people to prevent inevitable winter waves. Whilst the initial and booster COVID programmes succeeded in older adults, uptake was much lower in under 40s, and almost non-existent in young children due to delayed, confused and lacklustre messaging (Figure 2). I remain dumbfounded that we vaccinate kids for influenza, but not SARS-CoV2, despite prolific acute hospitalisations and 10s of 1000s of kids suffering from long COVID in the UK.
UK COVID booster offers are now highly limited after stringent narrowing of eligibility, set to preclude pregnant women from spring 2025. Targeted vaccination continues to mystify, and not just for COVID. Delayed kids chicken pox vaccines are compounded by bizarre older age eligibility, whilst new RSV jabs are confined to pregnant women and over 75’s, but not over 80s or babies, unlike the USA. Even resurgent seasonal influenza in 2022 and a larger UK susceptible pool wasn’t enough to expand or accelerate seasonal vaccine programmes. Damaging concomitant waves of COVID, influenza and RSV ensued.
Unlike endemic viruses, balancing the rapid evolution of SARS-CoV2 with population immunity will require both reduced transmission and improved vaccines, involving invariant targets and longer-lasting protection. Alongside relentlessly evolving subvariants, “saltatory” evolutionary jumps emerge periodically from chronic patients, resetting the immunological clock. Crowbarring COVID into an influenza mould doesn’t work it evolves far more quickly; hence, “current” COVID immunisations are based upon JN.1 from Christmas 2023…imagine doing this for influenza vaccines!
Figure 2. Coverage of English initial and booster vaccine campaigns by age group until Nov 2023. Source: Independent SAGE, courtesy of Bob Hawkins and Prof Christina Pagel (UK Government data).
3. Communicate
Despite understandable pressures during a crisis, confused messaging was a constant feature of the previous Government’s COVID response. For example, the pervasive subject of supposedly accruing herd immunity by infection made a huge impact in the media, not helped by the now infamous quote from Boris Johnson that that the UK should take COVID “on the chin”. Despite this being taken somewhat out of context and “herd immunity never being the official UK strategy, confirmed by Sir Chris Whitty speaking to the COVID inquiry, the lack of nuance in public debate, and the favouring of such a strategy by some in Government, resulted in a major mismanagement of public communications.
Tragically, this concept was taken to the extreme by those advocating for the virus to “let rip” to obtain herd immunity, despite this never occurring historically without vaccination. Whilst fundamentally flawed, this appealed to some in Government, and fringe advisors were drafted in to argue against SAGE guidance as cases rose again in autumn 2020, before vaccines. The ensuing wave and the drive to save Christmas was itself highly damaging despite last minute restrictions, and provided fertile ground (R>1) for the emergence of the Alpha VoC. The handling of this resurgence led to widespread public distrust of the government response.
Whilst the availability of vaccines then prompted a roadmap out of restrictions based upon four key criteria, the precise data and thresholds used to guide decision making were never clarified. Ultimately, dates became more important than data, culminating in “freedom” day, which went ahead despite soaring cases of the Delta VoC and an attempt by Boris Johnson and Rishi Sunak to avoid self-isolation guidance. Naturally, this represented the opposite of freedom for many. A delayed tokenistic response to the Omicron variant later that year continued the “rollercoaster” series of reactive, rather than proactive responses to the virus. Trust was further undermined by high profile government figures contravening their own COVID guidance and revelations around a widespread “party culture” at Number 10.
In addition to policy, failures to communicate how SARS-CoV2 is transmitted have had important consequences for how COVID has been managed. Airborne transmission (Figure 3) has featured consistently at the inquiry, supported by experts. Yet, the healthcare Infection Prevention Control (IPC) cell continues to dismiss airborne transmission, doubling down on droplet transmission and insisting that fluid resistant surgical masks (FRSM) are sufficient protection for staff versus FFP2/3 respiratory protective equipment (RPE). Unsurprisingly, we continue to experience unacceptable levels of NHS staff illness as well as patient endangerment. Why does NHS policy appear beholden to the politicisation of mask wearing, rather than scientific evidence and WHO guidance?
Figure 3. Illustration highlighting how improved indoor air quality can mitigate infection risks, generated using ChatGPT.
The new Labour government faces tough logistic and financial challenges to repair the damage done to the NHS since 2010, but our pandemic strategy simply must adopt a more preventative approach. Since 2020, Independent SAGE has sought to fill a gap in science communication around pandemic policy, and to provide a forum where scientists communicate with the public. This has led to demonstrable impact, including organisations pledging to improve indoor air quality and other measures. The Government must communicate that urgent change is needed, with long-term investment in surveillance, vaccines, therapeutics, and a paradigm shift towards cleaner indoor air, reducing the need for draconian measures during the inevitable next pandemic.