“Just the ‘flu” hampers our response to the current Covid pandemic and future pandemics
Prof Steve Griffin on why "just a flu" is such a dangerous phrase
The phrase “just the flu” has enraged me since COVID began as it pays neither SARS-CoV2, nor influenza virus, the respect they deserve.
This phrase, clearly aimed at normalising pandemic harms, effectively benchmarks flu, which causes 1000s of UK deaths annually, as “normal”. This is despite available vaccines, drugs, and hard-earned population immunity against the flu virus. Sadly, familiarity breeds contempt, or in this case, complacency.
The UK “living with” COVID response relies entirely on this premise of flu as a “normal” illness, crowbarring a COVID peg into an influenza-shaped hole. The result: an overstretched NHS enduring additional health burden with little extra resource.
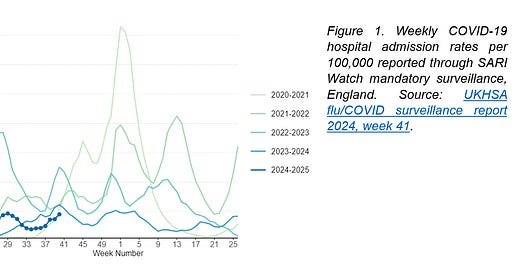
SARS-CoV2 has made “winter pressures” perennial (Figure 1). As a result, more people are dying, hundreds of thousands more people are unable to work, and support for Long Covid patients is dwindling. This “new normal” is NOT befitting of a country with (historically) advanced health and social care.
We are comparing two different chalks with two different cheeses…
We sometimes hear discussion of SARS-CoV2 “settling down”, becoming “endemic”, and – my personal favourite – behaving like “any other respiratory virus”.
This is disingenuous on at least two levels. First, it really hasn’t settled, and it shows no sign of doing so (Figure 2). Second, and perhaps most troubling, is the implication that SARS-CoV2, influenza, or other viruses, cause so little harm that they shouldn’t affect our lives.
What’s actually being discussed is predictability, with the implication that predictable means benign. However, virus transmission and disease depend upon the balance between virus and host, namely the capacity of the virus to evolve and transmit, versus immunity and our environment.
Figure 2. Prevalence of SARS-CoV-2 lineages amongst available sequenced cases for England from 2 October 2023 to 22 September 2024. Source: UKHSA flu/COVID surveillance report 2024, week 41.
The “R value”, familiar from Government COVID briefings, shows infections increasing when R (the Reproduction rate, or how many people an infected person infects on average) is above 1, or decreasing when R is below 1. When R is about 1, things remain stable, predictable, yet infections still occur if the baseline prevalence (infections over time) is high. Endemic flu and Coronaviruses have a low baseline with one, sometimes two, waves each year caused by newly susceptible kids, waning immunity, and behaviour/environment temporarily pushing R over 1, usually in winter.
Seasonality is more complicated than “people spending more time indoors”, I heartily recommend this review by Prof Akiko Iwasaki.
Even hardened sceptics would struggle arguing that SARS-CoV2 fits this pattern, given it is causing multiple waves annually since emerging in 2019. The balance still favours its fast-paced evolution outmanoeuvring immunity; any support from public health mitigations is now all but extinct.
The SARS-CoV2 evolutionary rate is 3-4 times that of the fastest seasonal influenza, H3N2. This is more to do with the virus tolerating change rather than mutating quickly, with the spike protein adapting for transmissibility and antibody evasiveness, seemingly without limits.
Essentially, this slippery virus successively creates new pools of susceptible hosts, driving new waves. Even now in 2024, we see concomitant epidemic waves across multiple countries; this, incidentally, is the definition of a pandemic. Virus evolution also “jumps” when highly mutated lineages emerge from immunocompromised hosts. This “saltatory” evolution occurred most recently for BA2.86, the forebear of JN.1 and the class of 2024. Once labelled “Variants of Concern” (VoC), this practice has now stalled, despite jumping immense evolutionary distances.
Whilst an emergent “pandemic” influenza would also tip the balance very much in its favour, influenza pandemics have historically caused one, two, or sometimes three large waves prior to establishing predictable, “endemic” behaviour. SARS-CoV2, the first Coronavirus pandemic of the modern era, simply doesn’t fit the influenza mould.
Even confronted with this, sceptics still retort: “doesn’t matter because COVID is mild”. I despair…
Viruses do NOT “just evolve to become mild”!
Misguided Australian rabbit folklore aside, this fallacy refers to disease, not viruses themselves, and is often false. Once again, the virus-host balance matters most. However, as individuals, each infection is a race and, if you run enough races, you can still lose, even with a head start from immunity.
Mercifully, we no longer see COVID hospitalisations and deaths on the scale of 2020/21, largely because vaccines accelerated our progress towards, and I mean towards, balance. Infection-induced immunity plays its part but is accompanied by far greater risk of harm and inherent survivorship bias. Depressingly, labelling this as “natural immunity”, like something from a health food shop, has led to profoundly misleading, tabloid-fuelled concepts like “immunity debt”. Please, just stop.
Nevertheless, the diminished individual risk of severe acute COVID is countered by uncontrolled prevalence at the population level. In addition to antibody evasive variants, our immunity vs. severe disease also wanes, but can be restored using well-matched boosters.
Boosters are critical for millions of erstwhile shielders and clinically vulnerable people, who usually mount poorer vaccine responses and are more likely to develop severe disease should they get infected. Whilst multiple boosters can help protect some patients, this is confounded by the high level of exposure due to now-skeletal vaccine programmes and poor mitigations. Hence, the trivialisation of COVID and other infectious diseases remains unjustifiable.
Shockingly, some proponents of “natural immunity” dubbed the ancestral Omicron variants of concern as “nature’s vaccine” in 2022, due mainly to their preference for the upper over the lower airway. While BA.1 and BA.2 were less acutely pathogenic in animal models, they caused the largest COVID waves of all time and did profound harm. Hospitalisations exceeded the pre-vaccine November 2020 peak and were double that of the Delta variant. England saw ~33K certificated COVID deaths during 2022, despite vaccines, and inherent virulence was clear from a devastating outbreak of BA.2 in poorly vaccinated populations of Hong Kong. Over time, Omicron subvariants have adjusted to both innate and adaptive immunity, with some regaining lower lung preferences and animal model pathogenicity. This appears to be happening again for BA.2.86/JN.1 derived lineages. Thus, severe disease is mainly countered by immunity, NOT viral attenuation.
So, the only way to slow a pandemic is to either improve immune longevity or slow down the virus, ideally both! For influenza, so far, we caught up relatively quickly, thankfully limiting the 1918 H1N1 “Spanish” influenza to just two waves, albeit at the cost of over 50 million lives. This is difficult to compare with prevalence-adjusted death estimates for COVID of 20-35M to date, due to duration, modern healthcare, vaccines, and therapeutics. Interestingly, the 2009 H1N1 “Swine flu” pandemic had comparatively lower impact due to cross-protective anti-H1N1 responses in older patients, derived against endemic offspring of Spanish influenza. Swine flu emerging just a decade later may have been far more devastating.
Despite familiar “winter pressures”, most of the public don’t take flu seriously enough. Over 10,000 deaths are attributed to influenza and pneumonia (ICD-10 codes J09-J18) annually. Consistent with good cross-protective immunity, only ~10% list seasonal influenza (J09 to J11) as underlying cause, compared with 50-70% for COVID; the main complication of influenza is secondary bacterial pneumonia, and this was also the case for Spanish influenza. Ultimately, despite the “with, not of”-ness throughout the pandemic, for anyone with a semblance of common sense the clinical impact of both viruses is a major issue. Years like 2018 when the flu vaccine match was poor were highly damaging, but again the pandemic balance tells; 1.4 million years of UK lives were lost to COVID in 2020 pre-vaccine, four to five times that for 2018 flu AND pneumonia.
Finally, whilst post-viral syndromes are not new, the sheer scale of long COVID is unprecedented (Figure 3). It is, by no means, “bollocks”. More than 2 million people in the UK alone continue to report suffering symptoms in 2024, including 10s of 1000s of children. Whilst acute severity increases risk, many cases follow mild infections. Sadly, many experience similar dismissive gaslighting encountered by ME/CFS patients over past decades. However, this is being countered by firm immunological and other markers of disease, although it’s recognised that long COVID has overlapping features with ME/CFS and some adverse vaccine reactions. Interestingly, for many people with Long Covid, ongoing symptoms appear linked to persistent SARS-CoV2 infection as well as reactivation of preexisting herpesviruses. Worryingly, other post-acute sequelae are now conclusively linked to SARS-CoV2, including cardiovascular, neurological, gastrointestinal, and metabolic diseases, including a worrying spike in juvenile onset type 1 diabetes.
Figure 3. Estimated global cumulative incidence of long COVID, based upon meta-regression estimates that pool together all available evidence. Source: Al-Aly, Z., Davis, H., McCorkell, L. et al. Long COVID science, research and policy. Nat Med 30, 2148–2164 (2024). https://doi.org/10.1038/s41591-024-03173-6
Recent vaccination reduces long COVID risk, plus some promising drug repurposing prospects exist. In fact, reinfection is associated with a cumulative higher risk of developing long COVID, because you can’t get Long Covid without getting Covid first. Sadly, despite recognised health, economic and societal impact, research and patient support in the UK has been downgraded. However, a clear lesson for future pandemics is to dovetail initial responses with mitigations against the long-term sequelae of infection.
As we continue to see warning shots from H5N1 influenza infecting birds, wild animals and currently US cattle, the frustration at this country’s continued inability to learn from mistakes and improve upon pandemic preparedness is tangible. We owe it to those who have been lost and continue to suffer to ensure that the same mistakes don’t happen again. This absolutely requires that we also reduce the harm done by existing endemic diseases whilst addressing health inequality across the UK. Back to normal simply isn’t good enough.